I wrote the following stories published by The Children’s Hospital of Philadelphia Research Institute in September 2016:
Tag: neuroscience
April 2016 Writing for The Children’s Hospital of Philadelphia
I wrote the following articles published by The Children’s Hospital of Philadelphia Research Institute in April 2016:
Restoring Balance in the Brain After Concussion
CHOP Oncologist Appointed to Blue Ribbon Panel for National Cancer Moonshot
Teaching a Computer to See Like a Dermatologist
Study Maps Early Connectivity Networks in Newborn Babies’ Brains
CHOP Research In the News: Transgender Youth, Vaccines, and Sleep
In Bench to Bedside: Finding Research Success in Setbacks
Growing Into Healthy Relationships: A Teen Dating Violence Q&A
CHOP Research In the News: Genetic Superheroes, Excess Bone, and Secondhand Smoke
Coordinating Research with 80 Million Participants: A PCORnet Q&A
Hakon Hakonarson Honored for Excellence in Research Mentoring
CHOP Research In the News: Plastic Bronchitis, Baby BMI, Voice at the Vatican
New Brain Study Tailored for Nonverbal Children on the Autism Spectrum
Originally published in Bench to Bedside, the CHOP Research monthly publication.
I composed this original article based on interviews with the investigators.
Excerpt:
The children who speak least — or not at all — are rarely represented in cutting-edge brain imaging research on autism spectrum disorder (ASD). Researchers at The Children’s Hospital of Philadelphia aim to change that with a new study enrolling children with ASD who are minimally verbal or nonverbal.
“This is really an underserved community who have not been given the opportunity to participate in research,” said Timothy Roberts, PhD, vice chair of research in the Department of Radiology at CHOP and a professor of Radiology at the Perelman School of Medicine at the University of Pennsylvania. “More importantly, the results of the research are not directly applicable to them, so even if we developed a drug for ASD impairments led by our biomarkers, we wouldn’t know if this treatment really was good for individuals with ASD with more limited verbal and cognitive ability.”
Dr. Roberts and colleagues from CHOP’s Center for Autism Research want to know whether certain aspects of neural rhythms and timing of neural firing that they found to be characteristic of ASD in previous studies, using noninvasive brain imaging called magnetoencephalography (MEG), are indeed common across the spectrum.
“When neural activity is happening, it produces electrical and magnetic fields,” said J. Christopher Edgar, PhD, a co-leader of the study and a clinical neuropsychologist and brain imaging researcher in the Department of Radiology at CHOP. “We use this machine to measure the magnetic field. We do that to look at brain function.”
The neural biomarkers that Dr. Edgar and Dr. Roberts have found correlate with the level of clinical impairment in the children they have studied to date, particularly in the realm of language ability.
“There is a scientific question: Does this correlation extend into this nonverbal and minimally verbal population in a continuous way, or is it a separate disorder?” Dr. Roberts said. “I suppose a fundamental question is: Is the autism spectrum continuous or discrete in terms of these brain markers?”
Proton Therapy Neuropsychology Study Receives Dissertation Award
Originally published on Cornerstone, the CHOP Research Blog.
I composed this original article based on interviews with the investigators.
Excerpt:
Babies being treated for brain cancer have not received traditional radiation therapy since the 1980s. At that time, doctors realized that the side effects of radiation hitting healthy developing brain tissues in very young children was simply too severe. But within the past decade, proton therapy has become available to some of even these youngest patients. This newer radiation therapy method has a more targeted radiation beam that better concentrates its effect on the tumor while hitting fewer healthy tissues — but the nature of its effects on the developing brain are still being studied.
One such study, a doctoral dissertation project by a researcher at The Children’s Hospital of Philadelphia, was recently recognized for its quality of design and potential impact with the John E. Gordon Dissertation Award from the Philadelphia Neuropsychology Society (PNS) and Clinical Neuropsychology Associates.
How Precision Medicine is Reshaping Epilepsy Research
Originally published in Bench to Bedside, the CHOP Research monthly publication
I composed this original article based on multiple interviews with the investigators.
Excerpt:
The little girl’s epilepsy was so debilitating that she was virtually nonresponsive. Traditional antiseizure medicines could not reduce the five to 20 seizures she experienced daily when she first came to The Children’s Hospital of Philadelphia.
Trying a new approach, her neurologist, David Bearden, MD, prescribed a drug that targeted a molecular pathway involved in her seizures, and within a month, she was seizure-free for the first time since a few days after her birth.
This success excited hope among epilepsy researchers worldwide that other such successful strategies could soon follow. The case exemplifies the popular concept of precision medicine, which is barreling ahead in cancer but not yet common practice in neurologic disorders such as epilepsy.
“Most drugs for epilepsy work like treating pneumonia with a cough suppressant: It may stop the symptom but doesn’t treat the underlying problem,” said Ethan Goldberg, MD, PhD, a CHOP neurologist and neuroscientist who was senior author of a case report about the little girl’s treatment (of which Dr. Bearden was first author) in Annals of Neurology in 2014. Her treatment, while not yet analogous to an antibiotic, was more precisely targeted to the underlying mechanism of her seizures than most treatments.
The future need for precision medicine is one that epilepsy researchers are approaching with conscious attention to the field’s strengths and unmet challenges. Dr. Goldberg was a presenter at a precision medicine scientific symposium during the American Epilepsy Society annual meeting in December. His colleague, Dennis Dlugos, MD, MSCE, a CHOP pediatric neurologist, was among the major contributors to an international consortium of researchers who authored a roadmap for precision medicine in epilepsy published in The Lancet Neurology this fall.
Drugs May Be What’s the Matter With White Matter in HIV
Originally published in Bench to Bedside, the CHOP Research monthly publication
I composed this original article based on an interview with the investigators.
Excerpt:
Some of the neurological and psychiatric complications associated with HIV may be side effects of the medications that control the virus, and not caused by the virus itself, according to a new study from researchers at The Children’s Hospital of Philadelphia and the University of Pennsylvania. Their pre-clinical findings were published in the Journal of Neuropathology and Experimental Neurology.
Certain antiretroviral drugs were associated with problems in developing myelin proteins in cell models and animal models, and the drugs were associated with reductions in white matter in autopsy brain samples from a cohort of individuals with HIV, reported the research team led by co-senior authors Judith Grinspan, PhD, research professor of Neurology at CHOP, and Kelly Jordan-Sciutto, PhD, chair and professor of Pathology at Penn’s School of Dental Medicine.
Both senior researchers emphasized that individuals with HIV should continue taking lifesaving antiretroviral drugs as prescribed. They hope their current and future findings can help researchers refine drug designs to reduce side effects, and help clinicians pursue prescribing practices that are risk-informed and tailored to the patient’s age and stage of brain development. These future changes could be particularly important for children with HIV whose brains are still developing.
Stroke Rehabilitation Research Connects Brain to Gait
Originally published in Bench to Bedside, the CHOP Research monthly publication
I composed this original article based on an interview with the investigator.
Excerpt:
If you have ever hit your stride on a moving walkway, the type commonly found in airports, consider how it felt when you stepped back onto solid ground. You may have felt a sudden but brief discombobulation while your brain worked to correct its temporary mismatch with your body’s sense of movement. Laura Prosser, PhD, PT, is trying to induce a similar reaction to rehabilitate children after stroke.
As a research scientist in the Division of Rehabilitation Medicine at The Children’s Hospital of Philadelphia, Dr. Prosser’s work is focused on how the brain and its connection to the body change after damage and during rehabilitation. Her focus on children addresses an under-researched area in rehabilitation.
“Understanding how rehabilitation can impact neuroplasticity is the most exciting aspect of this research to me,” Dr. Prosser said. “Not much of this work has been done in children. At CHOP we are in a unique position to understand how the brains of children respond differently to rehabilitation than the brains of adults who have had an injury.”
Dr. Prosser is now conducting a small pilot study testing physical therapy outcomes after pediatric stroke using high-tech tools including a split-belt treadmill and brain-stimulating technology called transcranial magnetic stimulation (TMS). She aims to learn which approaches seem most promising to pursue in future larger trials.
Studying the Brain’s Fundamental Drum Beat to Understand Autism
Originally published in Bench to Bedside, the CHOP Research monthly publication
I composed this original article based on an interview with the investigator.
Excerpt:
A drum beat coordinating brain activity and thus organizing the music of life emerges from deep inside the human brain. This electromagnetic neural pulse —eight to 12 beats per second — is known as the resting-state alpha rhythm.
“Alpha rhythms may be the most fundamental brain rhythm, involved in coordinating brain processes from those as simple as hearing tones and those as complex as consciousness,” said J. Christopher Edgar, PhD, a clinical neuropsychologist and brain imaging researcher in the Department of Radiology at The Children’s Hospital of Philadelphia.
Researchers have known for some time that electromagnetic (neural) brain activity is different in individuals on the autism spectrum. In a series of recent studies, Dr. Edgar and colleagues have shown that the resting-state alpha rhythm is stronger among individuals on the autism spectrum, and that stronger alpha rhythms are associated with more severe clinical symptoms.
With a new grant from the National Institute of Neurological Disorders and Stroke (NINDS) of the National Institutes of Health (NIH), Dr. Edgar will use state-of-the-art noninvasive brain imaging called magnetoencephalography (MEG) scanning to measure brain activities, including alpha rhythms, and magnetic resonance imaging to obtain structural brain measures in adolescents with and without autism spectrum disorder (ASD). He aims to find out why that metaphorical drum beat, setting the pace for the activities of other players or different parts of the brain, sounds different in children on the autism spectrum.
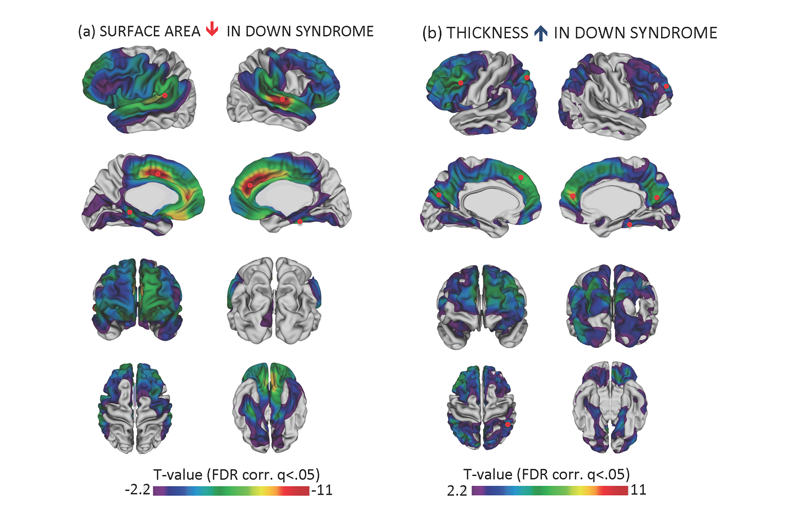
Thick Cortex Could Be Key in Down Syndrome
Originally posted on DrexelNow.
The thickness of the brain’s cerebral cortex could be a key to unlocking answers about intellectual development in youth with Down Syndrome. It could also provide new insights to why individuals with this genetic neurodevelopmental disorder are highly susceptible to early onset Alzheimer’s Disease later in life.
(more…)
Do Insect Societies Share Brain Power?
Originally posted on DrexelNow.
The society you live in can shape the complexity of your brain—and it does so differently for social insects than for humans and other vertebrate animals.
A new comparative study of social and solitary wasp species suggests that as social behavior evolved, the brain regions for central cognitive processing in social insect species shrank. This is the opposite of the pattern of brain increases with sociality that has been documented for several kinds of vertebrate animals including mammals, birds and fish.
“By relying on group mates, insect colony members may afford to make less individual brain investment. We call this the distributed cognition hypothesis,” said Sean O’Donnell, PhD, a professor in the Drexel University College of Arts and Sciences who led the study published today in Proceedings of the Royal Society B.
(more…)
